One night it occurred to me that something is very wrong with the set-up of the IV found in the bedroom at Michael's home. For starters, it was moved at some point in time. Besides that, other things do not add up when one looks at this IV stand and what was connected to it at various times. This issue ties somewhat into the issue of was there a gravity-fed propofol drip or not (which will be covered later). I think the best way to describe the inconsistencies is to use verbatim witness testimony from January, not October, with accompanying photos from the trial. I know there may be some changes in what these witnesses said in the trial but I will cover any differences later when those transcripts are available. The main objective of this blog is just to visually see the changes that occurred with this IV and see there is inconsistency.
The following testimony is from Alberto Alvarez:
When Alvarez made it to the second story of the home he states of Murray:
Alvarez: I SAW DOCTOR MURRAY COMING FROM LIKE A HALLWAY, AND HE WAS WALKING IN TOWARDS THE ROOM, SIR.
He states Murray was in the "Landing Area" and walking towards the "Foyer Area". Alvarez states Murray was "walking"--not running--towards the room.
Click on the photos to enlarge them.

Alberto states the only equipment he saw was an IV stand and oxygen tank. He states it was located on the far side of the bed, by the nightstand and the chairs.
Walgren: OKAY. AND COULD YOU TELL AT THAT TIME WHETHER THE I.V. STAND HAD ANYTHING ATTACHED TO IT AND THEN ATTACHED TO MICHAEL JACKSON?
Alvarez: WELL, I DIDN'T LOOK. I JUST -- I NOTICED IT WAS THERE. I DIDN'T FOCUS ON IT UNTIL I WAS GIVEN, I WAS TOLD TO GRAB SOMETHING FROM THERE.
Alvarez states Murray removed vials from the nightstand and placed them in a clear bag that Alvarez grabbed, located in or by a chair. Alvarez states at this time Murray was kneeling, not standing. Alvarez was at the foot of the bed. Alvarez was then instructed to place the clear bag with vials into a brown bag that was to the left of a chair that was facing the bed, right at the bottom. Alvarez states there was a blue bag next to the brown bag.
Walgren: NOW IN REGARD TO THE I.V. BAG REMOVAL, CAN YOU DESCRIBE WHAT DOCTOR MURRAY SAID AND DID IN INSTRUCTING YOU TO REMOVE THE I.V. BAG FROM THE I.V. STAND?
Alvarez: YES, FROM HIS POSITION, HE POINTED WITH ONE HAND TO THE I.V. STAND AND HE SAID, "REMOVE THAT, REMOVE THAT BAG AND PUT IT IN THE BLUE BAG."
Walgren: AND DID YOU NOTICE ANYTHING ABOUT THAT I.V. BAG THAT CAUGHT YOUR ATTENTION WHEN YOU REMOVED IT?
Alvarez: YES, SIR. THE I.V. BAG WAS HANGING MORE OF EYE LEVEL AND SO AS I AM REACHING TO DISCONNECT IT FROM THE TOP OR UNHANG IT, I NOTICED AT THE -- AND INSIDE, THERE WAS LIKE A BOTTLE INSIDE THE BAG. AND I JUST -- I NOTICED THAT AND THEN I NOTICED THAT AT THE BOTTOM OF THE BAG, THERE WAS LIKE A MILK-LIKE SUBSTANCE, SIR.
Walgren: OKAY. SEPARATE FROM THE BOTTLE, YOU ARE TALKING ABOUT A LIQUID?
Alvarez: YES. IT WAS AT THE TIP OR AT THE BOTTOM OF THE BAG, SIR.
Walgren: AND WHEN YOU SAY "MILK-LIKE," DO YOU MEAN COLOR? CONSISTENCY?
Alvarez: IT LOOKED LIKE MILK.

Walgren: AND WHEN YOU REMOVED THAT I.V. BAG, IT APPEARED TO HAVE A BOTTLE INSIDE OF IT. WAS THERE STILL ANOTHER I.V. BAG HANGING FROM THE I.V. STAND?
Alvarez confirms there was another bag.
Walgren: OKAY. DID DOCTOR MURRAY EVER INSTRUCT YOU TO REMOVE THAT BAG?
Alvarez: NO, SIR.
Walgren: OKAY. ONCE THE 911 CALL WAS CONCLUDED AND THE 911 OPERATOR HAD ADVISED YOU TO GET MICHAEL JACKSON TO THE FLOOR, WHAT DID YOU DO?
Alvarez: I WENT AND, I BELIEVE, I SAID WE GET HIM TO THE FLOOR. AND THEN I GRABBED, I GRABBED MR. JACKSON'S LEGS. BUT AT THAT TIME, I DIDN'T KNOW HOW TO GRAB BECAUSE THERE WAS AN I.V. STUCK IN HIS LEG AND DOCTOR MURRAY PROCEEDED TO TAKE IT OFF WHEN HE SAW THAT I WAS HESITATING AND SO I GRABBED HIS LEGS, AND HE GRABBED THE UPPER PART OF HIS BODY. AND BY -- WHILE HE WAS REACHING FOR THAT, HE ALSO PUT THIS APPARATUS IN HIS FINGER. AND THEN WE PROCEEDED TO BRING HIM DOWN TO THE FLOOR.
This apparatus was a pulse-oximeter. Alvarez had not seen it placed on Michael before but had seen the device a few days prior as Murray asked for batteries for it.
Chernoff: IT (the IV) WAS STILL CONNECTED TO MICHAEL JACKSON WHEN YOU MOVED HIM?
Alvarez: PRIOR TO US MOVING HIM, MR. CONRAD MURRAY REMOVED THE I.V.
(You will later see this statement by Alvarez clashes with that of Richard Senneff.)
Chernoff: OKAY. SO, AND THIS WAS JUST RIGHT BEFORE YOU MOVED HIM DOWN TO THE FLOOR?
Alvarez: YES, SIR.
Chernoff: AND I ASSUME THAT YOU HAD TO MOVE THE I.V. STAND AS WELL SINCE IT WAS RIGHT THERE IN THE WAY OF WHERE YOU WERE PLACING MICHAEL JACKSON?
Alvarez: I DON'T RECALL, SIR, BECAUSE IT WAS A LONG, PRETTY LONG TUBE, CLEAR TUBE THAT WAS CONNECTED TO THAT I.V. SO THE I.V. WASN'T IN THE WAY. WE JUST BROUGHT HIM DOWN RIGHT BESIDE THE BED, SIR.
Chernoff: NOW THIS I.V. BAG THAT YOU TOOK OFF THE STAND, THE I.V. STAND, IT WASN'T SUCH -- WAS IT A SITUATION WHERE YOU COULD JUST QUICKLY REMOVE THE I.V. BAG? OR WAS IT SITUATED WHERE YOU HAVE TO, KIND OF HAVE TO TURN IT AROUND TO CURLY Q. IT ON?
Alvarez: THAT IS CORRECT. I HAD TO CURL IT AROUND BECAUSE IT WAS A LITTLE HOOK LIKE THAT. SO.
Chernoff: SO YOU CERTAINLY HAD A PERIOD OF TIME WHERE YOU WERE HOLDING THAT I.V. BAG, CORRECT?
Alvarez agrees.
Chernoff asks if it had any fluid in it.
Alvarez: VERY LITTLE FLUID AT THE BOTTOM. AND THE ONLY REASON I NOTICED IT WAS BECAUSE IT WAS UP TO MY EYE LEVEL. I NOTICED AT THE BOTTOM OF IT, THERE WAS THAT MILKY WHITE SUBSTANCE, SIR.
Chernoff: WE ARE GOING TO GET TO THAT, BUT WAS THE ONLY FLUID THAT SMALL AMOUNT OF FLUID THAT WAS GOING INTO THE CONNECTOR?
Alvarez agrees.
Chernoff: WHERE WAS THAT BOTTLE THAT YOU SAW INSIDE THE I.V. BAG?
Alvarez: IT WAS TOWARDS THE BOTTOM OF THE BAG, SIR.
Chernoff: AND YOU ARE SURE TODAY IT WAS INSIDE THAT I.V. BAG, RIGHT?
Alvarez: TO MY BEST OF MY RECOLLECTION, YES.
Chernoff: THE I.V. BAG THAT YOU SAY WAS LEFT ON IT, ON THE STAND WAS THE ONE THAT WAS CONNECTED TO MICHAEL JACKSON? YOU REMEMBER THAT?
Alvarez: YES, SIR.
Chernoff: OKAY. THE ONE THAT YOU TOOK OFF FROM THE I.V. STAND WAS NOT CONNECTED TO ANYBODY OR ANYTHING?
Alvarez: NO, SIR.
Chernoff asks if it was just hanging there and Alvarez states this is correct.
Alvarez did note that he recalled seeing an ambu-bag (he referred to it as a breathing apparatus and said it was on the floor). Though there are no photos of the vial in the bag as it was seen by Alvarez or Fleak, Fleak did retrieve this vial from the cut bag. Alvarez stated the propofol was secured in the IV bag and slightly diagonal. This could have contributed to some of the propofol in the corner of the bag though some appears to be on the outside of the bag as well.

See here for some additional photos regarding Alvarez.
Now, we move onto paramedic Richard Senneff and his testimony about the IV set-up:
Walgren: DID YOU SEE AN I.V. STAND OR I.V. KIT?
Senneff confirms he did.
Walgren asks where the IV was located.
Senneff: THAT WAS ON THE SAME SIDE OF THE BED BETWEEN THE DOCTOR AND ME, YEAH.
Notice that Senneff states the IV pole was located on the same side of the bed as the nightstands, or the left/far side of the bed.
Walgren: NOW, LET'S TALK ABOUT THE I.V. STAND. YOU SAW THE I.V. AT LEAST WHEN YOU ARRIVED, THE I.V. WAS HOOKED UP TO THE PATIENT?
Senneff agrees.
Walgren: DO YOU RECALL WHERE IT WAS HOOKED UP TO?
Senneff: I BELIEVE IT WAS HIS LEFT LEG ON THE CALF, ON THE INSIDE OF HIS LEFT CALF.
Walgren: DID THAT APPEAR TO BE HOOKED UP TO A STANDARD SALINE BAG OR I.V. BAG?
Senneff: YES, IT DID. I DIDN'T EXAMINE THE BAG, BUT AT A DISTANCE IT APPEARED TO BE A STANDARD SALINE BAG.
Now, Alvarez stated that Murray removed the IV when they moved Michael to the floor. Given the IV catheter was still in place, it seems Murray disconnected the IV tubing from the bag to the catheter only, not the catheter itself (at least, not at that point in time). At some point then, it seems Murray reconnected the IV tubing though there is an overlapping of when Michael was being moved to the floor by Murray and Alvarez and when paramedics arrived in the bedroom. Murray would have had to have reconnected the IV fairly quickly.
Walgren: WHEN YOU GAVE THE FIRST ROUND OF EPINEPHRINE AND ATROPINE, WAS THAT ADMINISTERED VIA THAT I.V. THAT HAD ALREADY BEEN IN PLACE OR A NEW I.V.?
Senneff agrees it was already in place.
Walgren: WAS THERE SOME TYPE OF, I GUESS, RESTRUCTURING OF THE I.V. PORT THAT NEEDED TO BE DONE TO MAKE YOUR EQUIPMENT COMPATIBLE WITH THAT I.V.?
Senneff agrees and Walgren asks for a explanation.
Senneff: THERE IS TWO SYSTEMS FOR ADMINISTERING MEDICATIONS THROUGH I.V.'S. IT IS WITH A NEEDLE AND WITHOUT A NEEDLE, COMMONLY REFERRED TO AS NEEDLE-LESS. IN THE PRE-HOSPITAL CARE SETTING, WE CHANGED OVER TO A NEEDLE-LESS SYSTEM YEARS AGO BECAUSE IT IS JUST TOO EASY TO STICK YOURSELF WITH A CONTAMINATED NEEDLE WHEN YOU ARE DRIVING DOWN THE STREET IN THE BACK OF AN AMBULANCE. THE DIFFERENCE IS YOU HAVE THE I.V. CATHETER, THE TUBE THAT IS ACTUALLY IN THE VEIN. IT HAS A LITTLE HUB ON IT, THEN THE PORT THAT GOES INTO IT. THAT IS THE DIFFERENCE IS THE TYPE OF PORT. A NEEDLE PORT HAS LIKE A LITTLE RUBBER STOPPER ON THAT YOU PUT THE NEEDLE IN THE CENTER. A NEEDLE-LESS HAS A VALVE INSIDE. YOU SCREW THE NEEDLE-LESS SYRINGE ONTO IT, AND THEN THAT RELEASES A VALVE AND YOU PUSH THE SOLUTION IN THEN YOU UNSCREW IT TO REMOVE IT. WITH A NEEDLE, YOU SLIDE THE NEEDLE IN, INJECT SOLUTION, AND SLIDE THE NEEDLE BACK OUT.
Walgren: JUST TO BE REAL SIMPLE HERE, WHEN YOU GET THERE, THERE IS AN I.V. BAG HANGING FROM THE I.V. STAND?
Senneff agrees.
Walgren: A TUBE IS COMING FROM THAT BAG, AND IT IS ATTACHED TO MICHAEL JACKSON'S LEG AREA?
Senneff agrees.
Senneff states the bag was connected to Michael but as will be pointed out after all testimony is covered, the bag found at the scene may not have had tubing attached to it.
Walgren: THEN OFF OF THAT TUBE AT SOME LOCATION IS A PORT ALLOWING FOR THE ADMINISTRATION OF DRUGS INTO THAT I.V. TUBING?
Senneff agrees. Senneff states it was a needle system kit when he arrived.
Walgren: SO WHAT WAS CHANGED TO ALLOW YOUR SYRINGES TO SCREW IN, TO BE ACCESSED VIA THE PORT THAT ALREADY EXISTED?
Senneff: WE REMOVED THE SALINE LOCK ITSELF OF THE PORT SYSTEM. JUST CHANGE IT OUT. LEFT THE HUB IN AND PUT A NEW ONE IN.
Walgren: WHILE LEAVING THE EXISTING TUBE, I.V. BAG?
Senneff agrees.
Walgren: JUST CHANGED OUT THE PORT?
Senneff: YES. THE PORT IS WHERE WE ARE GOING TO BE INJECTING OUR MEDICATIONS.
Senneff is asked how many rounds of epinephrine and atropine he gave in the IV catheter in the leg. He states two rounds of each medication.
Walgren: AT SOME POINT THEN AFTER THESE TWO ROUNDS, DID THE LEG I.V. -- WAS IT COMPROMISED IN SOME WAY?
Senneff agrees.
Walgren: DID YOU SEE HOW THAT HAPPENED?
Senneff states he did. Walgren asks what happened.
Senneff: WE HAD OUR MEDICAL KIT OPEN. WE REFER TO IT AS A STARTER KIT. IT HAD THE MEDICATIONS THERE, THE COMMON CARDIAC MEDICINE THAT EVERYBODY IS FAMILIAR WITH IN THE BUSINESS. DR. MURRAY TOOK SOME OF OUR -- TOOK SOME OF THE MEDICINE, AND HE USED THE I.V. PORT AND INJECTED INTO THAT. BUT HE IS USED TO A --
Walgren tells him not to speculate what Murray is used to and asks him what he saw. It seems Senneff was going to speculate Murray was accustomed to a needle-based system only rather than a needleless one.
Senneff: IN USING IT, HE PULLED IT OUT. HE PULLED THE I.V. OUT.
After Michael was transported downstairs, Senneff went back upstairs to retrieve equipment.
Walgren: WHEN YOU WENT BACK UP THE STAIRS TO CHECK ON YOUR EQUIPMENT, DID YOU SEE DR. MURRAY UP IN THE ROOM?
Senneff states he did. Senneff is asked what, if anything, was he doing.
Senneff: HE WAS STANDING AGAIN ON THE OTHER SIDE OF THE BED HERE BY THE NIGHTSTAND AND HE HAD A BAG. I WANT TO SAY WHITE, LIKE A PLASTIC TRASH BAG TYPE THING. HE WAS STRAIGHTENING UP, PICKING THINGS UP.
Senneff did not say what Murray was picking up as he was not focusing on him that intensely.
Low (former attorney): AS YOU ARE LOOKING AT THAT SCENE, WERE YOU ABLE TO SEE IF THERE IS ANY MEDICAL LOOKING EQUIPMENT ANYWHERE AROUND?
Senneff states he saw the IV pole with the saline bag.
Low: WHERE, IN RELATION TO THE PERSON IN THE ROOM, IS WHERE THAT I.V. BAG IS?
Senneff: IT IS ADJACENT TO THE BED, APPROXIMATELY WHERE THE PATIENT'S KNEES ARE.
Low: ARE YOU ABLE TO APPROXIMATE DISTANCE INSIDE THE BEDROOM OR FROM THE PATIENT?
Senneff states it was within a foot.
Again, Senneff locates the IV was by the bed.
Paramedic Blount also gave his account of what he saw regarding the IV set-up"
Blount: HE SAID THAT THE REASON WHY THE PATIENT HAD THE I.V. BAG ATTACHED TO HIS LEG WAS BECAUSE HE REHEARSALED THE NIGHT BEFORE. HE WAS EXHAUSTED.
Blount also confirms an IV was attached to Michael as well.
Blount: IT WAS, I THINK IT WAS A HYPODERMIC NEEDLE HE CAME OUT WITH, AND IT WAS LIKE A BLUE COLOR. AND HE SAID, "YOU SHOULD BE ABLE TO USE THIS HERE." AND I THINK WE ALL SAID, NO, THAT IS OKAY.
This remark by Blount is a bit odd to me given it seems Murray had items, such as needles, directly on him, such as his pockets.
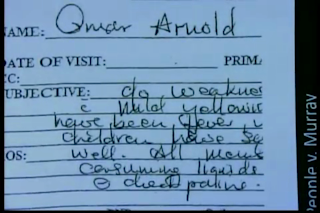
Michael was taken to the hospital. Coroner investigator Elissa Fleak went to the house that evening and spent about 80 minutes collecting evidence, mostly looking for "pills" as she stated. She did see the IV stand but did not pay any special attention to it at that time. It was not until June 29th, 4 days later, that the IV pole and what it contained was on it was inventoried.
Fleak: THE STAND IS THE METAL POLE WITH THE HOOK AT THE TOP. SALINE BAG IS HERE. THERE IS TUBING DOWN TO THIS AREA WHERE THERE IS A FORK OR A CLAMP IN THE TUBING WHICH HAS A SYRINGE IN IT THEN TUBING CONTINUES DOWN AND IS CLOSED.
Fleak states she entered the IV bag and IV kit into evidence on June 29th, 2009.
She states there was liquid in the IV bag.
Flanagan: AND THIS I.V. BAG HAD SOME TUBING COMING DOWN FROM IT?
Fleak agrees. However, photographs seen below would question her agreement to this statement:

Flanagan: IN THAT TUBING, THERE WAS A SYRINGE?
Fleak: HALFWAY DOWN THE TUBING, THERE WAS A CLAMP, A V-SHAPED CLAMP AND IN ONE OF THE HEADS OF THE CLAMP THERE WAS A SYRINGE. IT WAS NOT DIRECTLY IN THE TUBING.
Fleak is the first person to mention a syringe connected to the IV tubing, in any form. Recall Senneff stated that some portion of the tubing also had the valve changed from one that required a needle to one that did not. The syringe was connected to the tubing via the Y port built into the tubing using a needle. We know this syringe contained flumazenil, propofol and lidocaine as did the distal, short end of the tubing.


Fleak states she cannot recall if the tubing below the Y port had liquid in it but did recall clear liquid in the tubing above the Y port. She also states the bag was clear--no white substance. She states the IV bag appeared to be 3/4 full, 1/2 to 3/4 full when hanging.
Walgren: DID YOU ALSO RECOVER -- EXCUSE ME -- WAS THERE ALSO AN I.V. STAND WITH AN I.V. KIT ATTACHED TO IT AT THE SCENE?
Fleak: YES, THAT WAS IN THE ROOM. IF YOU ARE FACING THE BED, AT THE FOOT OF THE BED IT WAS TO THE RIGHT, TO YOUR RIGHT.
Walgren: IF YOU ARE AT THE FOOT OF THE BED LOOKING TOWARD THE HEAD OF THE BED, IT WOULD BE TO YOUR RIGHT?
Fleak: TO YOUR RIGHT.
Now we see at some point the IV stand was relocated. See the photo below to get a general idea of where the IV was at one point versus where it was later moved.




The golden curtains with the photo of a child in the chair is situated directly across from the bed. If you were lying in the bed, and lifted up, that is what you would see. If you looked to the left, that is where the IV pole had been moved, close to a set of drawers with photos. The chairs were between the bed and the closet/bathroom.
Criminalist Jaime Lintemoot examined the IV equipment and provided a diagram show below:

Walgren: BUT THIS IS A BASIC DIAGRAM OF THE I.V. KIT, INCLUDING THE I.V. BAG, AS WELL AS THE ACCOMPANYING I.V. PLUG, TUBING, THUMB CLAMP, WHITE CLAMP, A Y-FORK, AS WELL AS THE SYRINGE, AND THE SHORT TUBING?
Lintemoot agrees.
Walgren: LET'S JUST BEGIN THEN WITH ITEM "A" SHOWN IN THE TOP LEFT PORTION OF YOUR DIAGRAM. WHAT IS THAT?
She states item A is a diagram of the IV bag. She states it was not attached to the rest of the system at the time she received it for analysis. The particular bag used by Murray came from a company called Hospira. I called Hospira to ask if once a bag was spiked, would it leak once the spike was removed. Hospira confirmed that it would leak all contents once the spike was removed from the bag. Thus, it seems this bag seen by the paramedics, Fleak and Lintemoot was never spiked with IV tubing. Rather, the bag with the propofol bottle enclosed had been spiked and used for saline administration sometime prior to Michael's death, as well as prior to being slit and having a bottle placed in it. Recall that no propofol was found in the long tubing--only the short tubing which also had a syringe hanging out of it when found by Fleak. There was no mention of a syringe by Alvarez, Senneff or Blount.



Walgren: ON YOUR DIAGRAM THEN IN THE LOWER LEFT CORNER, THERE IS A LEGEND INDICATING WHICH ITEMS OR WHICH LABELS APPLY TO WHICH ITEMS?
Lintemoot agrees.
Lintemoot agrees to Walgren's reading of the the key or legend to her diagram. "B" is the syringe--consisting of barrel, plunger and needle. "C" is the "Y" connector. Lintemoot states she does not know if it was plastic or not.
Walgren asks for Lintemoot to describe the syringe and "Y" connector.
Lintemoot: IT WAS A "Y" CONNECTION PIECE. THE SYRINGE WAS GOING INTO ONE END, A PIECE OF SHORT TUBING COMING OUT THE OTHER END, AND A PIECE OF LONG TUBING GOING INTO THE THIRD END.
Lintemoot agrees that "D" is the short tubing that lies below the "Y" connection.
Walgren: AND THE SHORT TUBING THEN PROCEEDS TO "E," WHICH YOU LABEL AS CLEAR TIP. WHAT IS THAT?
Lintemoot: IT WAS A CLEAR TIP THAT HAD A LITTLE BIT OF RED FLUID OR RED STAINING ON THE END OF IT.

Lintemoot confirms "F" is the long tubing.
Walgren: WITH THE "Y" PORT OR THE "Y" CONNECTOR, YOU HAVE A SHORT TUBE COMING OUT OF THE BOTTOM, THE SYRINGE GOING IN THROUGH THE TOP, THEN YOU ALSO HAVE THE LONG TUBING COMING OUT THE THIRD AND FINAL PORT; IS THAT RIGHT?
Lintemoot agrees.
Lintemoot states "G" is a white clamp attached to the tubing and "H" is a white thumb clamp.
Lintemoot states "I" is an "IV bag plug" and describes it:
Lintemoot: IT WAS A CYLINDRICAL PIECE THAT THE LONG TUBING WAS ATTACHED TO WITH A SPIKE ON THE END. TYPICALLY, IT GOES INTO THE I.V. BAG.
It seems Lintemoot is actually referring to the spike and drip chamber as an IV bag plug which is something else which will be covered here shortly.
Lintemoote then covered the following:
Propofol and lidocaine were contained in 0.19 g (approx. 0.2 mL) of fluid from the syringe on the nightstand.
Propofol, lidocaine and flumazenil were contained in 0.17 g (approx. 0.2 mL) of fluid from the syringe connected via needle to the "Y" connection.
Propofol, lidocaine and flumazenil were contained in 0.47 g (approx. 0.5 mL) of fluid from the short IV tubing.
No medications were detected in 17 g (or about 20 mL) from the long IV tubing or 0.38 g (about 0.4 mL) of fluid from the saline bag.
Given the descriptions above along with the photos provided--the IV found in the bedroom at Carolwood was altered at some time by someone. Was it altered by Murray as Michael was being taken downstairs by paramedics? Was it altered by someone other than Murray? I am not sure. I can say that with the syringe being placed in the tubing as it were--it almost seems as if that was planted there as a distraction. Now, this would go against Murray wanting anyone to know he had ordered propofol, but propofol in the IV does not mean that Murray ordered, either. It could, however, have been a useful way to try and say Michael self-injected something. After all, Murray initially tried to claim Michael had his own supply of propofol which is a lie. I already covered in a previous blog the evidence excludes the possibility of Michael self-injecting anything on June 25th.
I know the experts during the trial (Drs. Shafer and White) battled it out over whether or not there was a drip utilized. However, this syringe found would seem to indicate that boluses, either with a drip or without one, were used. Why this was not highlighted clearly, I am not sure. Perhaps it is because boluses would place a person there witnessing any arrest whereas a drip would not (hence, the "involuntary" charge). At some point soon I hope to cover everything the experts said as I think both men should be given credit for their years of study though that does not mean everything stated by them is necessarily fact. With Murray being the only one who knows the truth--all anyone can do is try to guess at what he did to the victim, the victim being Michael in this case. I hope Murray thinks about releasing some details after his stint in jail--even if it is pointing the finger at others (besides Michael), maybe a portion of it will be true given he will be angry after some time that he is the only one who had to be "punished".